Surgical Weight Loss Options
Appointments
Your Surgical Weight Loss Options
The main goals of metabolic and weight-loss surgery are to:
- Help the patient achieve a healthier weight
- Reduce health conditions that are related to obesity and improve overall health. This happens because of weight loss and the impact of surgery on metabolic and hormonal pathways that are not working well in the body
- Extend life expectancy and quality of life
- Improve the patient’s self-image, confidence and psychological health
- Support long term healthy behaviors
At Lahey Hospital & Medical Center, we offer all types of metabolic and weight loss surgery. These include Roux-en-Y gastric bypass, sleeve gastrectomy, duodenal switch/single anastomosis duodenal switch and revisional surgery for weight regain, additional weight loss or complications from prior procedures. You will work with your surgeon and members of the multidisciplinary care team, to figure out what the best option is for you.
Nearly all of the weight-loss surgeries are performed laparoscopically or robotically. Laparoscopic and robotic surgery are completed through 5-6 small incisions, as opposed to the large surgical opening used in traditional surgeries. Performing surgery this way cuts down on complications and speeds up your recovery time. Sometimes, some patients are not candidates for laparoscopic or robotic surgery. For these people, the procedure is done through a traditional open surgery.
Gastric bypass is the surgery that has been around the longest for weight loss. It involves surgically separating the stomach so that a small pouch is created at the top. The small bowel is divided and connected to this pouch, completely bypassing the portioned-off section of the stomach and about 150 centimeters of the small intestine.
The gastric bypass works in several ways: First, it creates a much smaller receptacle for food, preventing you from overeating. Second, because it bypasses a section of intestine, it reduces the intestinal area that absorbs nutrients and calories. Third, this surgery alters the stomach and intestinal hormones, reducing hunger and helping to fix diabetes in many people. Based on current research, this is the best weight loss surgery option for people with diabetes.
Weight loss is usually fairly rapid following a gastric bypass procedure; the average person loses about half of their excess body weight in the first six months. After that, weight loss slows down and finally reaches a plateau after about two years. Overall, patients lose an average of 60-70 percent of excess body weight. This means that if you are 100 pounds overweight, you can expect to lose about 60-70 pounds after gastric bypass and keep it off.
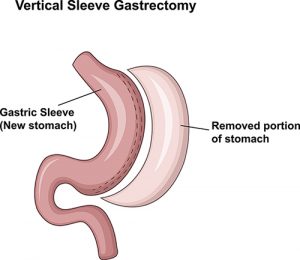
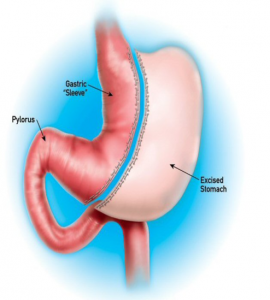 The most common procedure we complete at our facilities is the laparoscopic sleeve gastrectomy. Initial weight loss from the sleeve gastrectomy is a little less than the gastric bypass at one year.
The most common procedure we complete at our facilities is the laparoscopic sleeve gastrectomy. Initial weight loss from the sleeve gastrectomy is a little less than the gastric bypass at one year.
In this operation the outer part of the stomach is permanently removed. This decreases the amount of food that the stomach can hold by about 90%. The smaller amount of food that can be eaten passes more quickly into the intestine which is not surgically altered. Removing part of the stomach and speeding the delivery of food to the intestine changes intestinal hormones, decreasing appetite and improving diabetes.
The sleeve gastrectomy provides some advantages, namely no anastomoses (connections between the stomach and intestine) and no need to divide or bypass the intestine. This results in less risk of long term complications following this surgery compared to the gastric bypass.
The sleeve gastrectomy can make heartburn or reflux worse and is less effective in curing diabetes compared to the bypass. In those patients, gastric bypass is usually advised.
The most powerful procedure to lose weight is the laparoscopic duodenal switch. This procedure is not commonly performed, and reserved for individuals with obesity, typically those with a body mass index (BMI) of 50 or higher. It is also associated with a higher complication rate, so people that have a lot of medical problems are usually not good candidates. However, it is associated with 80% excess weight loss and the highest success with eliminating and preventing complications associated with obesity. In this operation, a sleeve gastrectomy is combined with an intestinal bypass to result in a combination of restriction and malabsorption. The overall hospital stay and recovery is the same as with the bypass and sleeve gastrectomy, but long term complications of diarrhea and vitamin and mineral deficiencies are higher.
Revisional surgery may be an option for patients who have already undergone a weight loss operation and have a problem that needs to be corrected. This can also be an option if they have regained weight, have lost an insufficient amount of weight or have increased difficulty with controlling diabetes.
 About 90% of the patients that have the Lap Band do not lose enough weight, regain weight or develop other problems such as reflux or difficulty swallowing. In these patients, the band can be laparoscopically removed, and a gastric bypass or a sleeve gastrectomy performed instead. The hospital stay and recovery is similar to non-revisional surgery. These operations are frequently performed at Lahey Hospital with excellent results.
About 90% of the patients that have the Lap Band do not lose enough weight, regain weight or develop other problems such as reflux or difficulty swallowing. In these patients, the band can be laparoscopically removed, and a gastric bypass or a sleeve gastrectomy performed instead. The hospital stay and recovery is similar to non-revisional surgery. These operations are frequently performed at Lahey Hospital with excellent results.
About 25% of patients can develop acid reflux after a sleeve gastrectomy procedure. Some patients may find this hard to control with medication or not want to remain on medication for the rest of their life. For these reasons, a patient may have revisional surgery and switch to a gastric bypass to improve acid reflux control.
Obesity is a disease caused by many factors. It is possible to regain weight after a sleeve gastrectomy surgery for many different reasons. Our team is here to help prevent this. However, if you have struggled with weight regain following a sleeve, you may be a candidate for a conversion to a duodenal switch/single anastomosis duodenal switch to help achieve greater weight loss. Some patients may also choose this type of surgery if they have poorly controlled diabetes or newly developed diabetes after a sleeve gastrectomy and would like to get better control with a surgery.
Weight regain can occur after gastric bypass surgery. Studies have shown that 15-35% of patients who have had gastric bypass do not achieve the expected weight loss or experience significant weight regain in the years after their surgery.
The limb distalization procedure can be a surgery to help reverse weight regain after bypass. This is an option for some patients, but not all patients who have regained their weight.
When this surgery is completed the area of absorption of nutrients in your small intestine is made shorter, which helps you to lose more weight. In the picture below you can see that there is a shorter area of intestine with purple arrows, which is where food and digestive juices are mixing and your nutrients are being absorbed.
When undergoing this surgery, patients have experienced an average drop in BMI by 11 points or have lost 62% of the excess weight on their body (ex: 100 pounds overweight = 62 pounds of weight loss). This can also lead to improvement in diabetes.
This operation, commonly known as “stomach stapling,” was very popular in the 1980s. In about 50% of patients the staples failed, leading to poor weight loss, stomach ulcers and pain. This operation can be converted to a gastric bypass.
This operation is necessary if there is a complication such as a fistula or connection between the bypassed stomach and stomach pouch. This can also lead to poor weight loss and ulcers. In other cases if the gastric pouch was much too large, weight loss will be inadequate and the pouch can be made smaller.
Frequently Asked Questions
Most patients will lose around 50 to 70% of their excess weight and keep it off for more than five years. That means if you are 100 pounds overweight, you can expect to lose 50 to 70 pounds in the first year after your surgery.
Yes. Over half of patients with type 2 diabetes no longer need any medication, and 90% require less medication after surgery.
Most surgeries last between two and three hours. Since all of our surgeries are performed through small incisions, patients only spend one or two days in the hospital. Most return to work after about one to three weeks, depending on the nature of their jobs.
We complete over 300 weight loss surgeries every year. Our surgeons, nurse practitioners, dietitians, operating room staff and other members of the team are highly skilled at delivering the best care and safest surgery.
We are accredited as a Comprehensive Center for Bariatric Surgery through the Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP).
To receive this accreditation, we have to demonstrate that we can take care of the most complex patient cases and deliver high-quality results. Representatives from the MBSAQIP program review our facilities, program and all other aspects of your care every three years to make sure we have everything we need to provide the best care possible.
Around a quarter of patients who undergo a metabolic or weight loss surgery may experience weight regain in the years following surgery.
Since there are so many factors that lead to obesity, causes for weight regain can vary based on the individual. Certain medications, exercise frequency and stress levels are all possible factors. Our team is here to provide long-term support to help prevent and reverse weight regain.
Yes. Our advanced practice providers or surgeons will talk to you about your weight-loss medication options. Additionally, if you’re struggling with weight gain after surgery, our team will evaluate your situation to determine whether medication is necessary. Our practitioners are trained to prescribe a wide array of weight loss medications.
All medical treatments, including surgery, have risks. However, the risk of mortality from obesity-related problems is higher than the risk associated with obesity surgery.
- More common are the risks of both short- and long-term non-fatal complications. (Overall there is a 10-20% risk).
- The most common short-term complications are nausea and dehydration (roughly 5-10%). Less common are bleeding and blood clots, each with risks around 1% or less.
- Long-term complications depend on the type of surgery. Patients that have the lap band experience band slippage, band erosion or intolerance of the lap band roughly half the time or more, which may require additional surgery.
- Patients that have the bypass might experience ulcers, bowel blockage, or vitamin and mineral deficiencies.
- Roughly 20% of patients that have the sleeve gastrectomy experience heartburn.
